2-Deoxy-d-glucose is a type of glucose that has had the 2-hydroxyl group substituted for a hydrogen atom, blocking it from being further broken down by glycolysis. To study its effects, 2-Deoxyglucose that has been marked with tritium or carbon-14 is used in animal models. It is then tracked by slicing the tissue and seeing where it goes under autoradiography observation. This may also be done with either traditional or electron microscopy.
The cellular glucose transporters are responsible for the uptake of 2-DG, so tumor cells which take up more glucose also tend to get in more 2-DG. Consequently, 2-DG has been proposed as a tumor therapeutic, and is now in clinical studies. However, the exact mechanism by which it impedes cell growth is quite uncertain; even though it appears to inhibit glycolysis it is insufficient to explain why cells cease to grow when exposed to 2-DG.
Due to its resemblance to mannose structurally, 2DG can stop N-glycosylation in mammalian cells and other organisms, thus activating ER stress as well as the Unfolded Protein Response (UPR) path. You can find 2-DG in 2dglab shop.
Use in optical imaging
2 deoxyglucose (2-DG) that has been utilized to identify targets through fluorescent in vivo imaging. Fluorodeoxyglucose is utilized in clinical medical imaging, such as Positron Emission Tomography (PET) scanning, in which one of the two-hydrogens in 2-deoxy-D-glucose is supplanted by the positron-radiating isotope fluorine-18. The emission of the paired gamma lines allows for imaging of the distribution of the tracer with the help of an exterior gamma camera. Nowadays, it is regularly done in coherence with a Computed Tomography (CT) aspect of the same PET/CT apparatus to permit better localization of the minuscule volume in tissue glucose-uptake disparities.
It is possible that India will use an approach with regards to treating COVID-19 that is similar to its strategy for Dengue.
On May 8th, 2021, the Drugs Controller General of India gave its approval for a pill form of 2-deoxy-D-glucose to be used in an emergency context as an adjunctive therapy for moderate to severe COVID-19 patients. The drug was developed with the assistance of the DRDO and Dr. Reddy's Laboratories, with the two groups declaring through a press release that the medication "has the potential to result in faster healing for those hospitalized and decrease the need for supplemental oxygen." However, both The Wire and The Hindu reported that the approval was based on weak evidence, with no journal publications or preprints available detailing its safety or efficacy.
Abstract
2-deoxy-d-glucose is able to disrupt d-glucose metabolism, highlighting the potential of energy and nutrient cramping in suppressing tumor growth and survival. Acting as an equivalent of d-glucose, 2-DG is processed into 2-deoxy-d-glucose-6-phosphate and accumulates in cells, which blocks hexokinase and glucose-6-phosphate isomerase and results in cell death. Apart from glycolysis hindrance, many other molecular mechanisms are also disrupted by 2-DG. In the current review, studies to enhance 2-DG’s drug-like features, its role as a compound to facilitate other chemotherapy drugs, as well as fresh 2-DG derivatives as potential anticancer agents are then detailed.
Aerobic Glycolysis in Cancer Cells
Tumor growth has been found to occur faster than the diffusion of oxygen can keep up with. For this reason, tumors are known to cause the production of new blood vessels via angiogenesis. This blood vessel formation is known to be leaky and instable, resulting in imbalanced oxygen levels and lactic acidosis. To be able to handle these changes, cancer cells have adapted the ability to function with anaerobic metabolism instead, to provide ATP and generate glucose-6-phosphate. Scientists believe the aerobic glycolysis process is advantageous to tumor growth, due to the cell biomass it produces, the precursors for fatty acid and nucleic acid it supplies, and the glucose it synthesizes, even in the presence of oxygen.
In reaction to the lack of oxygen, tumor cells re-modify their protooncogenes (e.g. the cellular myelocytomatosis oncogene (c-Myc)), adjust their signaling pathways (e.g. Phosphoinositide 3-kinase (PI3K/Akt)), and activate certain transcription factors (e.g. hypoxia-inducible factor 1 alpha, HIF-1α). This HIF-1α transcription is an essential factor in reformatting the metabolism of cancer cells. Usually activated during periods when food is scarce, HIF1α controls the transcription of genes for glucose carriers and glycolytic enzymes, strengthens mitochondrial respiration by increasing the production of pyruvate dehydrogenase kinase 1, and promotes mitochondrial autophagy. Additionally, HIF-1α maintains the equilibrium between oxygen utilization and production of ATP and dangerous ROS. Recreating oxidative metabolism as aerobically generated glycolysis is an indispensable system assisting in the survival and growth of cancer cells under hypoxic circumstances.
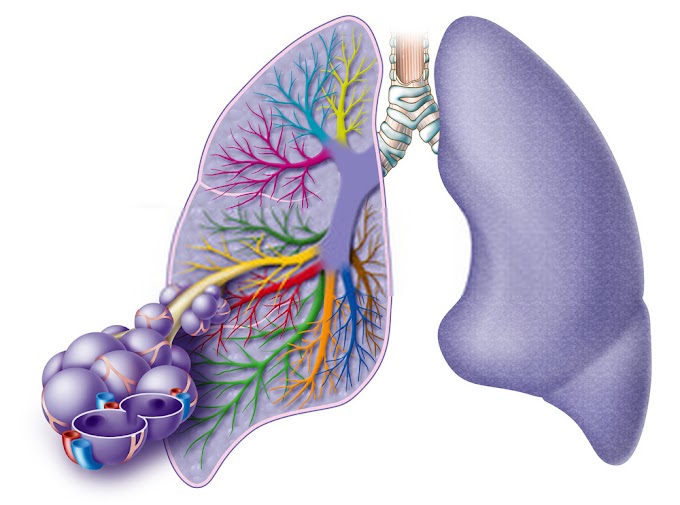
The GLUT glucose transporters allow the glucose molecule to enter the cell. The substance is then phosphorylated by hexokinase 'til it is changed into glucose 6-phosphate. It is then transformed to fructose-6-phosphate via phosphoglucose-isomerase (PGI) and phosphofructokinase (PFK). This second process occurs with the help of ATP and is allosterically inhibited by an abundance of the molecule. It is noteworthy since it oversees the overall procedure of glycolysis. Furthermore, it can be either engulfed in the pentose phosphate pathway (PPP) or remain as glucose-6-phosphate.
F-1 6-BP can either be converted into glyceraldehyde-3-P or dihydroxyacetone phosphate which are both utilized for the production of phospholipids and triacyloglycerols. Following this, phosphophenol pyruvate (PEP) is changed to pyruvate by the enzyme pyruvate kinase (PK). In human beings and other mammals, there are four isoforms of PK that are dissimilar in terms of their primary structure, kinetic functions, and expression in specific tissues. These are pyruvate kinase muscle isozyme M1/M2 (PKM1/PKM2), red blood cell PK (PKR), and liver-type PK (PKL).
The PKM2 isoform is a "paradigm", which is found in fetal tissues, stem cells, and in cells that are increasing in size, such as cancer cells. In normal cells, PK helps to regulate gluconeogenesis, a metabolic pathway in the liver that turns pyruvate, lactate, and other molecules into glucose when the body is low on food. When PK is deactivated due to the action of glucagon (normally during a state of food shortage), PEP is not transformed into pyruvate, and instead is switched to glucose as part of gluconeogenesis which is then circulated around the body to obtain food during deprivation.
The enzyme PKM2 has been found to be particularly active in tumor cells due to its ability to enable rapid glucose processing, thus fueling the development of cancerous cells. Also, under both oxygen-rich and anaerobic conditions, the enzyme LDH can be employed to convert pyruvate to lactate, while simultaneously oxidizing NADH to NAD+. As such, glycolysis can continue without requiring oxygen, as is seen in cancer cells. A diagram illustrating this phenomenon of aerobic glycolysis in cancer cells is provided.




0 Comments